The science and psychology of managing chronic pain
Chronic pain is one of the more difficult aspects of living with FSHD, and also one of the most challenging to manage. In various studies, between 82 and 89 percent of people with FSHD reported having significant pain, with 19 percent rating their pain level as “severe.” In this video from our FSHD University webinar, neurologist Kathy Mathews, psychologist Krista Kohl, and physical therapist Shelley Mockler explain that multiple factors go into an individual’s experience of pain. Consequently, they say that patients and their healthcare team need to develop a multi-pronged strategy to manage pain.
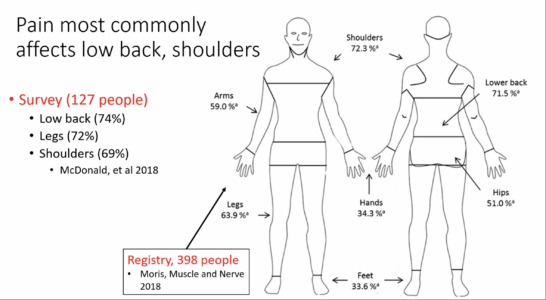 People report pain in many areas of the body, most frequently in the shoulders and lower back. There’s no single source or type of pain, and the level of pain bears no relationship with disease severity, age, or genetics.
People report pain in many areas of the body, most frequently in the shoulders and lower back. There’s no single source or type of pain, and the level of pain bears no relationship with disease severity, age, or genetics.
Dr. Mathews advises individuals seeing a pain specialist to “describe the pain in as much detail as you can. What makes it better or worse? When does it occur?” She emphasized that “pain is experienced in the brain,” and that this is a very important principle because “you can’t treat pain without involving the brain.” This by no means implies that pain is “all in the head,” but that focusing solely on the aching body part is often not sufficient, especially in chronic pain.
Dr. Kohl described the biopsychosocial model of pain, which involves linkages between chronic pain with such symptoms as depression, anxiety, and post-traumatic stress disorder. Pain can interfere with sleep, which in turn sets off a negative feedback cycle of fatigue, mood, activity, and energy. Understanding these links can help identify ways to intervene, she said.
 The team emphasized that the treatment of chronic pain is most successful when you use multiple approaches. This image of “What’s in your cup” suggests some key contributors to pain–and ways to address them. How can you build a bigger cup to be able to manage pain? Can you change your environment to remove pain triggers or reduce painful movements?
The team emphasized that the treatment of chronic pain is most successful when you use multiple approaches. This image of “What’s in your cup” suggests some key contributors to pain–and ways to address them. How can you build a bigger cup to be able to manage pain? Can you change your environment to remove pain triggers or reduce painful movements?
Remedies such as exercise, massage, electrical stimulation, foam rollers, and medications, provide relief that is short-term, but that may be enough to help re-set the negative feedback loops. A good physical therapist can be a key ally. “Think of your PT as a coach, not as someone who will ‘fix your pain,'” counseled Shelley Mockler. “Look for someone willing to learn.”
Webinar Slides (downloadable)
Resources
- Why Do I Hurt? – A Patient Book About the Neuroscience of Pain, by Adriaan Louw. Check out reader reviews to determine if this one is for you.
- The Explain Pain Handbook Protectometer, by David Butler and Lorimer Moseley.
- Mindfulness for Beginners: Reclaiming the Present Moment and Your Life, by Jonathan Kabat Zinn.


I am 80 yrs old. How do I relieve my hip & back pain. Also I cannot walk very far (30 ft.)
So glad to listen to this post! I am currently in pain and have been for several months, in the care of my primary doctor. Not sure if I injured myself more than just normal pain wise as Iifted a 63 pound dog and have been in pain ever since. No one mentioned whether I might should see an Orthopedic doctor for an injury with shooting pain and burning. I have an appt with my primary care Dr in a few days and will ask.
My daughter has FSH Muscular Dystrophy. It was diagnosed when she was 14. She is now 34 and her total lack of energy and increased pain is becoming evident. She also is psychophrenic and I think which makes this extremely hard for her. Her life source was adderall. It helped her so much but she has been taken off of it. It is pretty devastating. Can you help?
Hi Cathy, we’re sorry to hear about your daughter’s health challenges. In addition to FSHD, has she been diagnosed with schizophrenia(?), and perhaps ADHD (hence the Adderall)? Based on the guidance in this webinar, your daughter should be under the care of a multidisciplinary team including a psychiatrist, psychotherapist, and physical and/or occupational therapist. It would be important for them to have an understanding of her multiple conditions and how they might interact. It would be important to understand why she was taken off of Adderall, if this was done abruptly, causing withdrawal symptoms, and whether it is intended to be temporary. Her situation is very complex to manage. I hope you’re in an area where your daughter has access to multidisciplinary care.
I suffer from FSHD and have same fatigue and that medication being helpful I’m 33 as well and I believe is just the progression of the Disease. My mother has it as well and has the same symptoms yet worse. Almost feels like narcolepsy. Just wanted to reply and let you daughter know she is not alone. Take care friend