There are already many effective interventions
by Nicol Voermans, MD PhD, Radboud University Medical Center

We hear that currently there is “no cure for FSHD,” but this does not mean there is no treatment. Treatment and cure are two different things. There are many treatments already for FSHD. Indeed, most of the drugs being developed are not a cure but a treatment.
A treatment leads to an improvement in health, but it may not eliminate the disease, which is what a cure is. Medical professionals use medicine, therapy, surgery, and other treatments to help lessen the symptoms. That’s what we’ve been doing for a long time with FSHD.
A cure, on the other hand, usually refers to complete restoration of health. If you think about an infectious disease, your immune system eliminates the infection. Or you take an antibiotic and cure the illness. If you fracture a bone and your bone heals, you are cured.
A lot of diseases cannot be cured but can be treated very well. For example, diabetes cannot be cured in many patients, but there are effective, lifelong treatments for diabetes.
As you wait for new medicines, you should use the many treatments already available to manage your symptoms and help you live a better life. These are important not only for your current health status, but also because this is an essential part of preparing for participation in upcoming clinical trials. We call this “trial fitness.”
We clinicians work on designing better clinical trials. We call this “trial readiness.” As patients, you can contribute to this effort by becoming as trial-fit as possible.
Multidisciplinary, personalized care
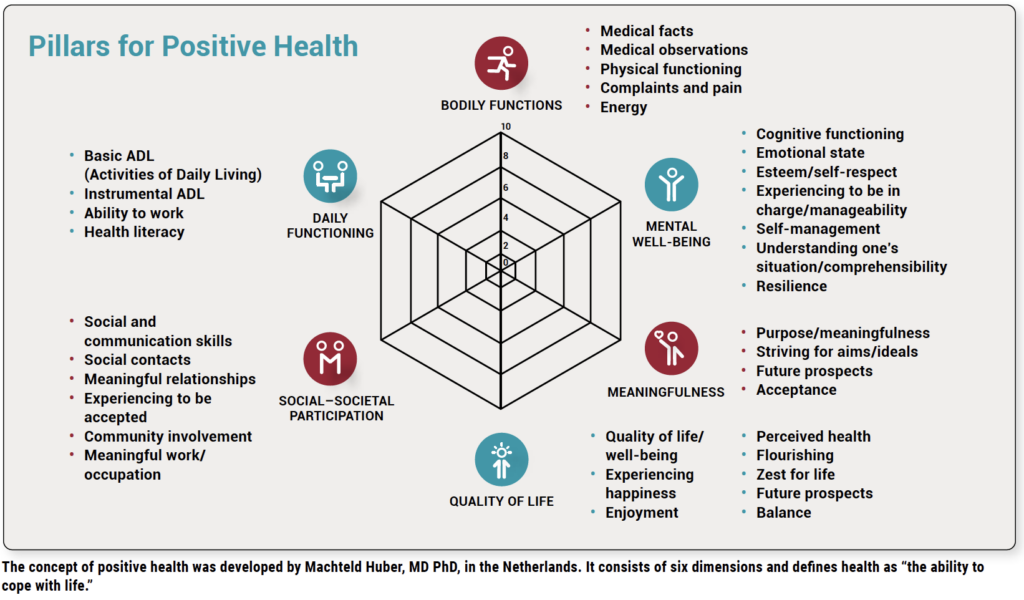
FSHD is more than a disease. It’s a condition that causes an individual to feel unwell. But the feeling also reflects the social consequences of having this condition. There’s an external and public aspect of sickness that involves society (see figure below).
The new drugs that are currently being developed for FSHD are directed against the genetic defect or the toxic DUX4 protein, or the downstream effects that damage muscle.
A patient with FSHD experiences the consequences of this muscle damage, such as pain, chronic fatigue, sleeping difficulties, physical inactivity, and reduced social participation. We have treatments to address these consequences.
Treatments should be personalized. What might be a problem for one person might not be an issue for another. So when thinking about treatment, you must ask yourself, What is the problem I am having? What does FSHD prevent me from doing, and what is the most important goal I can reasonably expect to reach?
Good treatment for FSHD is multidisciplinary. In my center in the Netherlands, we have an FSHD clinic set up by a rehabilitation doctor. He or she collaborates with the physical therapist, occupational therapist, speech therapist, psychologist, dietician, and social worker. Our neuromuscular nurse practitioner calls the patients two or three weeks before the appointment and asks, What are your current questions? The visit is then dedicated to the issues the patient would like to address.
Breathing and cardiac care
At our clinic, we assess respiratory strength in FSHD patients. The simplest way is spirometry. The test looks at the volume and velocity of air blown out of the lungs. Typically, in neuromuscular disorders, there’s a reduced strength of the respiratory muscles, which results in a reduction of “forced vital capacity” (the maximum amount of air you can exhale). This should be measured while sitting up and also while lying down (the latter because the diaphragm will move up a little bit as you don’t have gravity to help you push the abdominal contents down).
People with weakness of respiratory muscles will develop symptoms of hypercapnia (too much carbon dioxide in the blood) when lying down. This causes shortness of breath when lying down or bending forward, reduced sleep quality, and morning headache. You may be tired or fall asleep during the day. This is caused by a disturbed sleep pattern because if your carbon dioxide is not eliminated sufficiently, the body will wake slightly during the night. You will not wake up completely, but you won’t reach the deep phases of sleep, and that will cause all of these symptoms during the day.
That’s why it’s vital to test lung function even when patients don’t report symptoms of breathlessness during the day. In FSHD, approximately 40% of patients in wheelchairs or with scoliosis develop respiratory weakness to a degree that support is necessary.
Cardiac screening is also performed when a patient establishes care with a doctor. With FSHD, we don’t usually see any abnormalities in the heart muscle, so cardiac ultrasound is generally normal.
The electrocardiogram (ECG), on the other hand, may show abnormalities in the rhythm of the heart. There might be a delay in the conductance of the electric signal, which is called right bundle branch block. In general, this doesn’t cause symptoms and is not progressive. If it is detected, it will be followed up a year or two later. Patients are informed about it so if an ECG is made in another situation, they’re at least aware that they have this.
Chronic pain and fatigue
Treatment of chronic pain and fatigue is a topic to raise with your physical or occupational therapist. There’s very useful information on pain management by Dr. Katherine Mathews and her colleagues (see FSHD Society YouTube).
Nicole Voet performed a study 10 years ago of home exercise several times a week and cognitive behavioral therapy aimed at increasing physical activity in daily life. The results showed that with both interventions, compared to no intervention, patients became more physically active, slept better, had less fatigue, and were more able to participate in social activities.
Another project in our rehabilitation department was the “energy self-management program” for patients with various neuromuscular disorders. Researchers treated 29 severely fatigued people with different disorders for a month of self-management treatment, and 24 people received usual care. This study showed that people in the self-management program improved in walking. They were better able to endure physical activity and had better social participation, and these effects were sustained even after 11 months.
Many patients who participated in these studies said that the social support of other participants in the group was very helpful even years later.
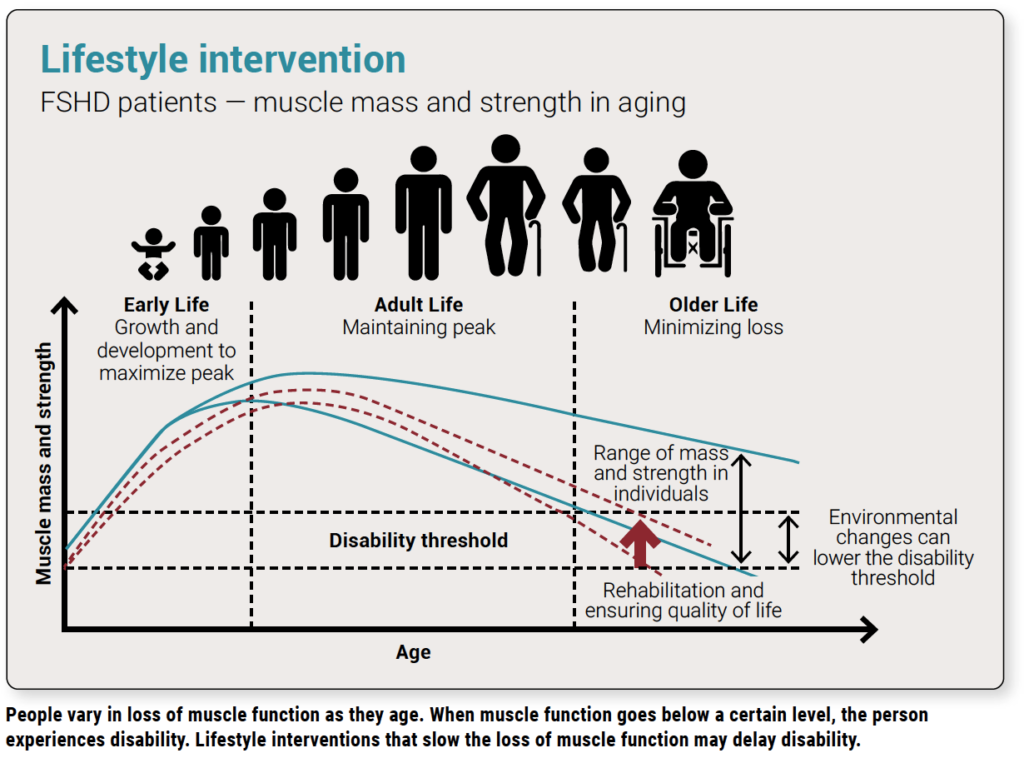
Lifestyle interventions are also very critical. As a typical person grows into adulthood, muscle mass and strength increase and then stabilize. At about 30 to 35 years of age, muscle strength starts to decline.
There’s a large range in muscle mass and strength among individuals, related to genetic factors, disease, and lifestyle. A person with FSHD might be less strong than other people, but they could actually be a bit stronger than someone with an unhealthy lifestyle or conditions such as diabetes or chronic lung disease.
With lifestyle interventions, you aim to give yourself a bit of an advantage (see figure below). Although it might not seem like much, it’s important to pay attention to it. I ask my patients, What aspects of your lifestyle can you change in the next few years? Which changes could be sustainable? What help do you need? No one will have a perfect lifestyle, but you can always think of something you can change for the better.
Mental and social well-being
Wellness involves mental and social health as well as physical health.
Often, adolescent patients are reluctant to see a psychologist because they don’t think they have a problem. I tell them, if you go to the physical therapist to train your muscles, why not go to the psychologist to train your thoughts? They can also become stronger with training. One of the approaches our psychologists use is ACT (acceptance and commitment therapy; see FSHD Society YouTube).
We also look at facial weakness and communication. We performed a study on the consequences of facial weakness on communication and social participation. We invited many patients to participate, but the average age of the participants was about 52 or 53.
Younger people were reluctant to participate and described facial weakness as upsetting. Older people said when they were younger it was difficult, but it became less of a problem as they became more self-confident and developed relationships. But they would have liked to have had support for this when they were teenagers. With the popularity of selfies, I think facial weakness might even be more of an issue for young patients today.
Facial expression is something we should consider as part of the multidisciplinary treatment with a speech therapist. Not only does it affect communication, but there are many ways to compensate for it. We are thinking about how to develop these insights into group therapy.
Care for children with FSHD
Children with symptoms before age 10 may have a more severe form of FSHD. They have a higher risk of hearing loss and abnormal blood vessels in the retina of the eye. They should have regular hearing and eye exams. It’s critical to catch these issues. Early intervention can prevent vision loss and delays in learning language.
A small subset of children have a very severe form of FSHD which is present before the age of five, but there are also children with a family history of FSHD who are diagnosed early. They may have fatigue, or not be able to smile, run well, or close their eyelids, but have no other visible disability. Yet these children have difficulties in school. They try to keep up with the physical capacities of their peers, but they can’t. It’s an invisible handicap. You cannot see it, but they encounter it daily.
It’s essential to support these children. Our pediatric rehabilitation department is doing a great job with them, and I hope their methods will become available in other countries.
FSHD affects entire families, and an important aspect of care is genetic counseling. This includes talking to family members and understanding different reproductive options.
Lastly, I always talk with patients about the precautions to take for a medical emergency. If you get into an accident and the medical responders don’t understand FSHD, or you’re unconscious, the doctor might use inappropriate medication for general anesthesia, so it’s important to carry a medic alert card. You can find them online; print them out and carry them in your wallet. You can also download an ICE (In Case of Emergency) app and enter the relevant information.


Bună ziua !Sunt din România și aș vrea să știu dacă primiți și din altă țară la clinică dv ? Menționez ca avem FSHD
Bună ziua, în prezent, medicamentul este disponibil numai prin studii clinice. Există multe studii care se desfășoară în Statele Unite și în întreaga lume. Puteți afla mai multe și puteți găsi încercări pe această hartă: https://www.fshdsociety.org/therapeutic-accelerator/ctrn/
Fabulous article. Thanks so much for the detailed information. This will be helpful for so many people with FSHD who don’t have access to a multidisciplinary team or specialized FSHD clinic. We can share this information with local neurologists, GPs etc as we so often have to advocate for ourselves and educate them on FSHD.
Thanks so much for sharing your knowledge and multidisciplinary model.
Good day
Could you advise if there is a FSHD clinic in the Uk and their details so i could contact them.
Thank you
Hello! There are two clinical trial sites in the UK: The University of Sheffield and University College of London. You can find more information, including site coordinator emails, on the map on our Clinical Trial Research Network page: https://www.fshdsociety.org/therapeutic-accelerator/ctrn/
Hi, very good article, thank you! Do you know of any clinic in Italy that embrace this multidisciplinary approach?
Thank you!
Are there any Fshd clinics in the Chicago area?